Benign Liver Tumours, Masses and Cysts - Assoc.Prof.Dr. Mutlu Unver Izmir, Turkey
- Doç.Dr.Mutlu Ünver
- Mar 20, 2024
- 4 min read
Benign liver tumours and cysts are quite common and can occur at any age. They are usually more common in young women. Such tumours include liver haemangioma, focal nodular hyperplasia (FNH) and hepatocellular adenoma.
Birth control pills, especially those containing estrogen, and pregnancy can increase the risk of hepatocellular adenoma. Liver cysts may be single or hydatid (echinococcus) cysts. Benign liver tumours and cysts are usually asymptomatic and are often detected incidentally during abdominal imaging.

However, in some cases (e.g. large lesions), symptoms such as upper abdominal pain or bloating after eating may occur. The diagnosis is usually made by imaging, but a biopsy may be required if the condition is uncertain. Treatment is usually conservative; surgery may be necessary only for certain types of lesions and in the presence of symptoms or complications.
Epidemiology and Gender Relationship of Liver Tumours:
Epidemiology
Prevalence: Hepatic haemangioma is the most common, followed by focal nodular hyperplasia (FNH) and hepatocellular adenoma is the rarest.
Gender: Generally more common in women than in men.
Hepatic haemangioma: Occurs in one male for every five females.
FNH: Occurs in one male to every eight females.
Hepatocellular adenoma: Occurs in one man for every nine women.
Age: Liver haemangioma is usually most common between 30-50 years of age.
FNH: It can occur at any age, but is more common in young women and is diagnosed in men at an older age.
Hepatocellular adenoma: More common in young women, usually between 15-45 years of age. Usually found incidentally during imaging tests.
Benign Liver Tumours Symptoms
In many cases, benign liver masses are usually asymptomatic and are usually detected incidentally during routine medical tests or imaging examinations.
However, in some cases, larger benign liver tumours can cause symptoms such as abdominal pain or discomfort, especially if they press on other organs.
Rarely, large benign tumours can lead to jaundice (yellowing of the skin and eyes) due to compression of the bile ducts.
Diagnosis of Benign Liver Tumours Symptoms
Benign liver masses are usually detected during imaging examinations such as ultrasound, tomography, MRI or routine check-ups.
When a liver mass is found, additional tests can be performed to determine whether this mass is benign or potentially cancerous. These additional tests include a liver biopsy, in which a small sample of tissue is taken and examined under a microscope to confirm the diagnosis.
Benign Liver Tumor Treatment
Most small benign liver masses usually do not require treatment and can be monitored with regular imaging studies as long as they do not grow or lead to complications.
If a benign liver mass is causing symptoms or there is uncertainty about its nature, treatment options may include surgical removal of the tumour (resection) or, in some cases, destruction of the tumour with minimally invasive techniques such as radiofrequency ablation (RFA) or microwave ablation (MWA).
In some cases where the benign tumour is extensive and cannot be safely removed by other treatment methods, liver transplantation may be considered.
Incidence:
The incidence of benign liver masses may vary according to tumour type and population. In general, these masses are often detected incidentally during other medical tests.
For example:
Focal Nodular Hyperplasia (FNH): FNH is one of the most common benign liver tumours. It is usually diagnosed in young and middle-aged adults and is more common in women than in men. The incidence of FNH in the general population is estimated to be approximately 3-5%.
Hepatocellular Adenoma (HCA): HCA is another benign liver tumour. The incidence of HCA varies depending on risk factors such as oral contraceptives or anabolic steroids. For example, the incidence of HCA is higher in women using oral contraceptives and is estimated to be approximately 3-4 cases per 100,000 women.
Liver Haemangioma: Liver haemangiomas are the most common benign liver tumours and are usually found incidentally during imaging studies. Their prevalence increases with age and they are found in approximately 5% of adults. Most of the time they do not cause symptoms and do not require treatment.
It should be noted that the incidence rates mentioned above are approximate and may vary in different populations and regions. It should also be noted that advances in medical imaging technology have led to more of these tumours being detected and more cases being diagnosed incidentally.
Regular check-ups, imaging studies and scans can help detect and monitor these benign liver masses and allow for timely treatment if necessary. If you are concerned about liver health or specific symptoms, it is important to consult a healthcare professional for appropriate evaluation and guidance.
Diagnostic Studies to Differentiate Benign Liver Tumours
Diagnostic Studies | Liver haemangioma | Focal nodular hyperplasia (FNH) | Hepatocellular adenoma |
Ultrasonography | Usually well circumscribed, homogenous, hypoechoic (pale) Image | 1.Homogeneous, hypoechoic to isoechoic structure 2.Round/oval, sharply circumscribed 3. central, star-shaped wound (∼50% of cases) | 1.Generally isoechoic Image 2. No obvious vascularisation 3.Heterogeneous due to haemorrhage 4. It is more common in the right lobe of the liver |
Contrast-enhanced ultrasonography | 1.Peripheral nodular healing in the early arterial stage 2.Portal venous and completely central filling in the late stages 3.Iris aperture phenomenon | 1.Rapid central or mixed filling in the arterial phase 2.Hypervascularity compared to neighbouring liver tissue 3.Sustained increase in the delayed phase or poor flushing | |
CT scan with contrast | 1.Good limited 2.Intermittent, nodular or peripheral healing in the early arterial phase 3.Subsequent gradual improvement towards the centre (iris diaphragm phenomenon) 4.Delayed phase hyperintensity due to contrast retention | 1. Increase in early arterial stage. Image 2.Hypointense 3.Portal venous phase isoentense and poorly visualised 4. Central wound ("vascular socket") | 1.Well determined 2.Heterogeneous density due to the presence of fat, glycogen and haemorrhage products 3.Peripheral healing in the early arterial phase due to feeder arteries 4.Sequential centred recovery pattern 5. No retention of contrast due to arteriovenous shunt in delayed phase |
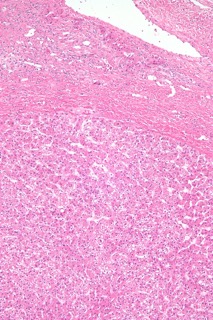
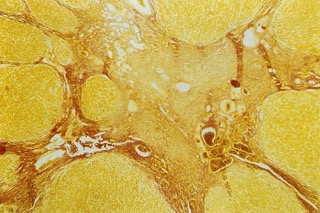
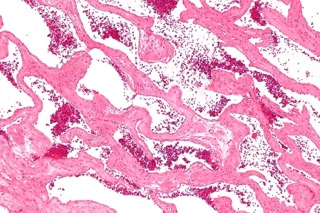
Pathology | 1. Cystic lesions of dark colour, possibly with stalks 2. Cavernous vascular spaces of variable size lined with smooth endothelial cells. Image | 1. Light yellow colour image compared with the surrounding liver tissue 2. Centrally located hepatocyte nodules with large impaired arterial branches and central fibrous tissue (central star-shaped scar) 3. May resemble macronodular cirrhosis | 1. Normal liver lobular architecture is absent. 2. Enlarged hepatocytes, image with small and regular nuclei 3. Cytoplasmic glycogen and lipid deposits 4. They are organised in layers or in cords 2 cells thick. |
Frequently asked questions (FAQs) about benign tumours in the liver
How is a benign tumor in the liver treated?
Most benign liver tumour do not require treatment. However, as we mentioned, in some cases, treatment can be performed with surgical operation, radiofrequency ablation or other minimally invasive methods (requiring less surgical intervention).
Over how many cm are liver cysts dangerous?
Simple liver cysts usually do not pose any danger. However, cysts of 4-5 cm or more may require follow-up and larger cysts may pose risks such as rupture or infection.
What causes a mass in the liver?
The exact causes of benign liver masses are not known exactly. However, genetic factors, hormonal imbalances, drug use and some health conditions may play a role in their formation.
How to recognise a benign mass in the liver?
Imaging methods (ultrasound, CT, MRI) and, if necessary, biopsy are applied to determine whether the masses are benign or not. In imaging, the structure, size and shape of the mass are examined.
Will the mass in the liver go away?
Generally, benign masses do not disappear spontaneously. They require follow-up, but they are harmless as long as there is no change in the size or structure of the masses.
Does a mass in the liver cause pain?
Benign liver masses usually do not cause pain. However, as the mass grows, it may cause a feeling of fullness, pressure or pain in the abdomen.
How are the liver masses removed?
The term "clearing a mass" is not exactly correct. While small and harmless masses do not require treatment, problematic masses can be completely removed surgically or destroyed by methods such as radiofrequency ablation and cryotherapy.






















Commentaires